Knowledge of Men’s Health Dangerously Low
Amongst British adults, urology diseases such as testicular cancer and prostate cancer are not well understood and men are not looking out for the signs… Read More

Amongst British adults, urology diseases such as testicular cancer and prostate cancer are not well understood and men are not looking out for the signs… Read More

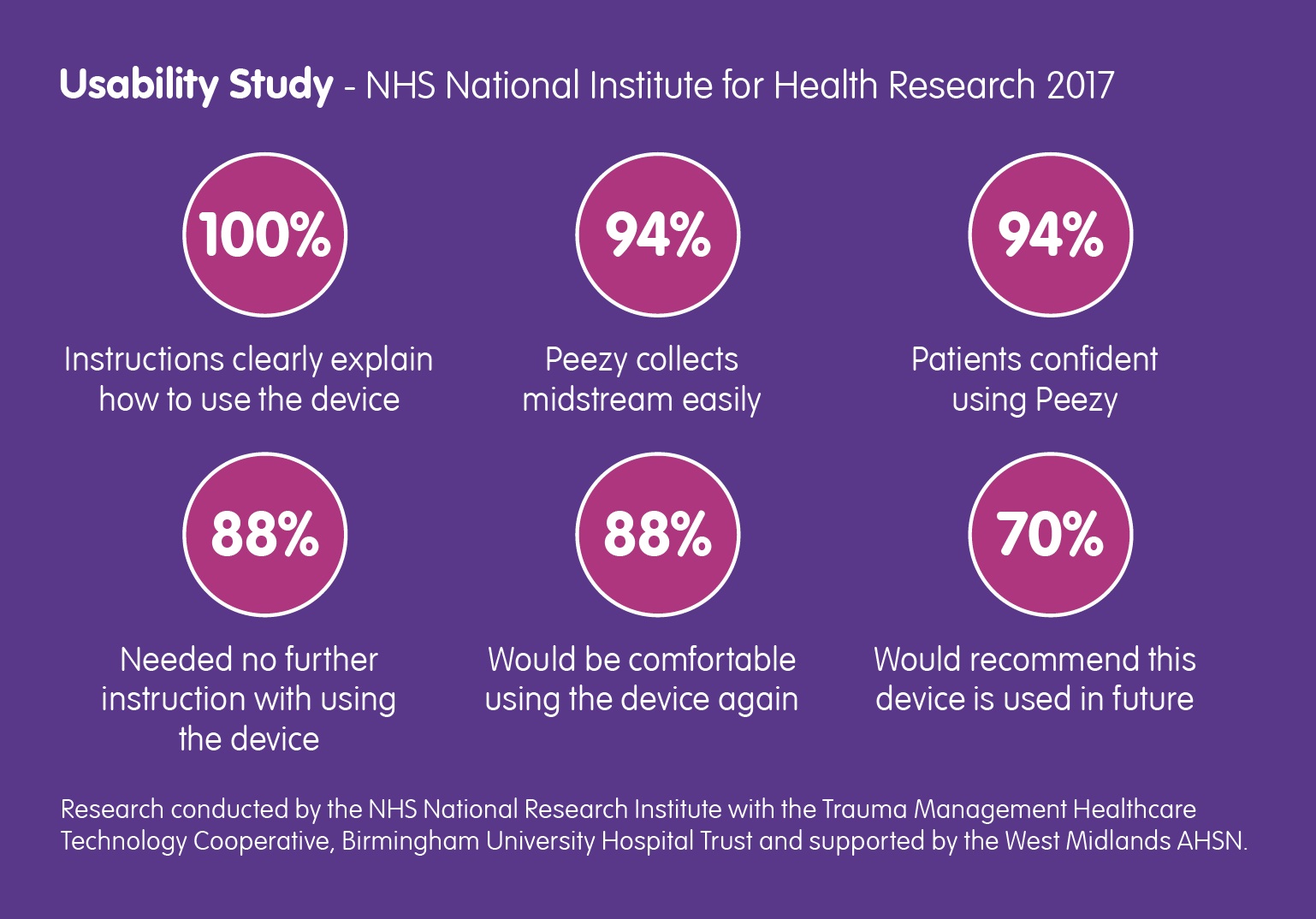
Back in March of this year, the NHS National Institute for Health Research contacted Forte Medical, asking for a case study… Read More
We’ve been an advocate for the MUST Campaign since they launched in May and this article explains why it is so important. Read about it… Read More

The inaugural speech delivered by Mr Matt Hancock upon his appointment as Secretary of State for Health, focused quite rightly on the… Read More
Barry Shrier, Founder of annual health innovation event Giant Live, presents the third Disruptor Giant Health Innovators TV interview featuring Giovanna Forte, CEO of Forte… Read More

In elderly patients, a UTI can induce behaviour that may be interpreted as “challenging”. As millions of us know, UTI is at best uncomfortable, at… Read More
Symptoms of urinary tract infections can be acute and in many cases, very debilitating. The need for a protocol around the collection of urine specimens… Read More
How easy is Peezy? Very! Click here to see our new animation showing five simple steps that deliver right-first-time urine specimen collection. Any clinician… Read More
Doctors can tell a lot about your health from your urine sample, if taken properly. Insightful piece by Rob Eley and Michael Sinnott from The… Read More

Encouraged by the growing national recognition of the value of urine in diagnostic medicine, health leaders are being approached to join a new Forte Medical… Read More
