Peezy Midstream Case Study at NHS NIHR Conference 2018
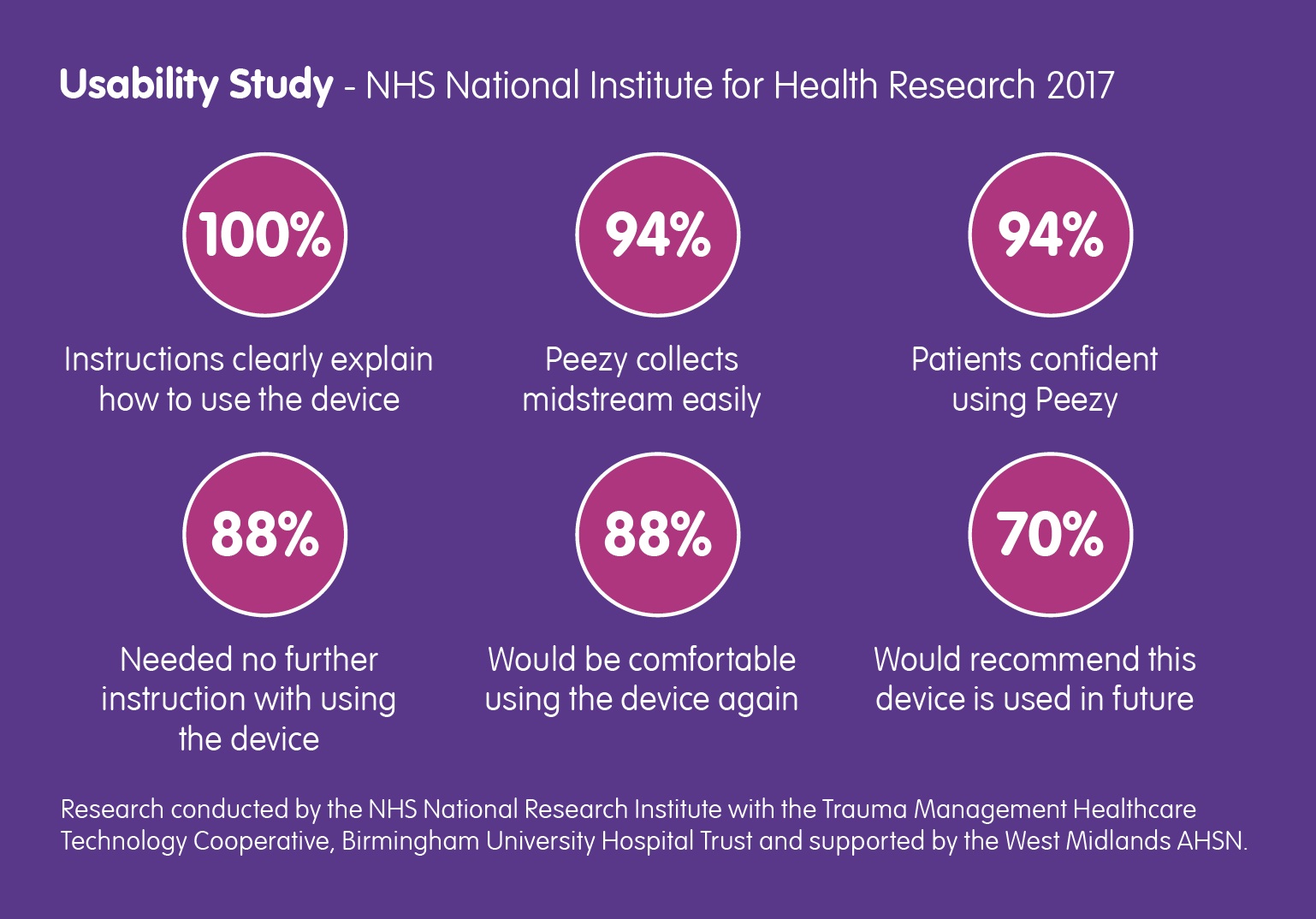
Back in March of this year, the NHS National Institute for Health Research contacted Forte Medical, asking for a case study… Read More
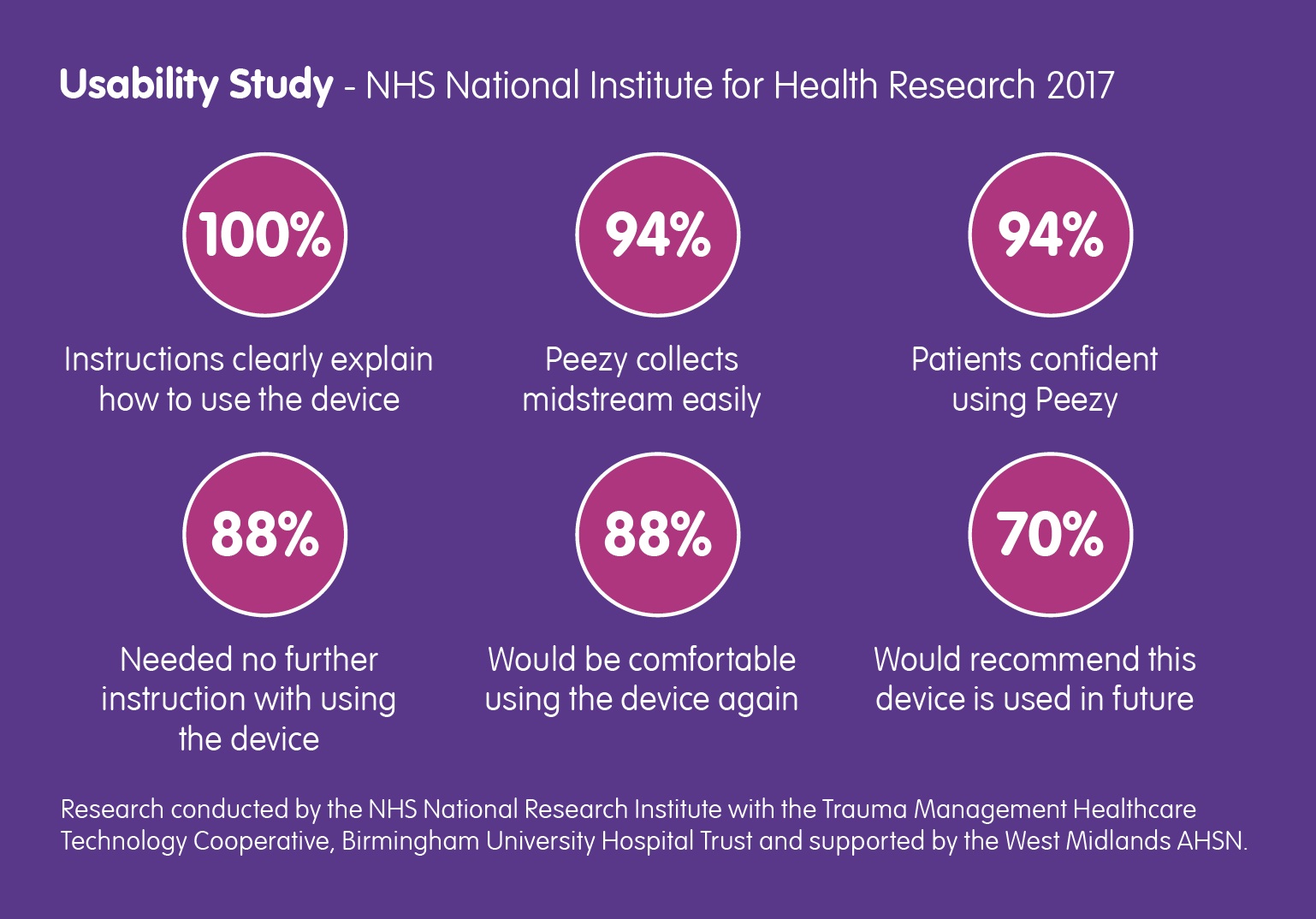
Back in March of this year, the NHS National Institute for Health Research contacted Forte Medical, asking for a case study… Read More
This is the latest recommendation following publication of a Californian study about the rise of antibiotic-resistant bacteria. But right-first-time diagnosis and treatment is only… Read More

A new study shows that Antibiotic-resistant UTI bacteria is becoming more common; Knowlex has created a short-film about the research and what you should know… Read More
The inaugural speech delivered by Mr Matt Hancock upon his appointment as Secretary of State for Health, focused quite rightly on the… Read More
Barry Shrier, Founder of annual health innovation event Giant Live, presents the third Disruptor Giant Health Innovators TV interview featuring Giovanna Forte, CEO of Forte… Read More

Antibiotic resistance in children’s E. coli, a bacteria that is the most common cause of urinary tract infection, is high against many antibiotics commonly prescribed in… Read More

An advocate and active player in healthcare infection prevention, we will participating at the Knowlex Infection Prevention and Control 2018 exhibition being held on Wednesday, 21st February… Read More

We have been talking prevention for some time so are pleased to see this report from Public Health England advocating right-first-time devices. Read the… Read More

From AMR to UTIs, independent participants at this year’s Forum highlighted the clinical and financial case for a “gold standard” urine specimen collection process that… Read More
The appointment of Andrew Turner as Business Development lead has brought new life to the introduction of Peezy Midstream technology to a number of leading… Read More
